MKSAP Quiz: Evaluation for increasing fatigue
An 81-year-old man is evaluated for increasing fatigue. He has no other symptoms to report. Medical history is significant for diabetes mellitus and hypertension. He does not drink alcohol or smoke. Medications are metformin and lisinopril.
On physical examination, vital signs are normal. The examination is unremarkable.
Laboratory studies:
| Hemoglobin | 8.5 g/dL (85 g/L) |
| Leukocyte count | 3100/µL (3.1 × 109/L) with 35% neutrophils, 45% lymphocytes, 20% monocytes |
| Mean corpuscular volume | 105 fL |
| Platelet count | 120,000/µL (120 × 109/L) |
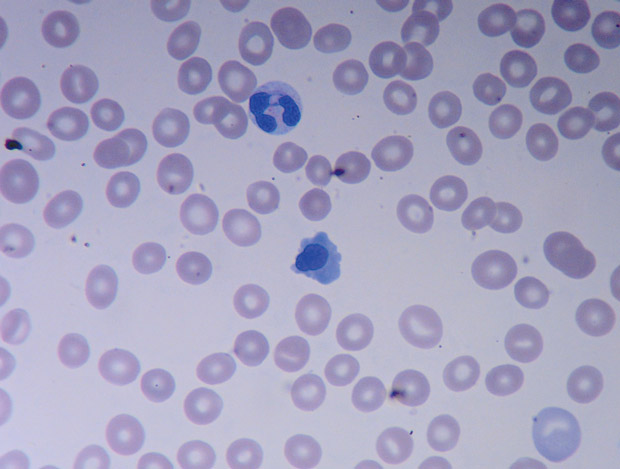
Serum levels of vitamin B12 and folate are normal. Peripheral blood smear is shown.
Which of the following is the most appropriate diagnostic test to perform next to evaluate this patient's anemia?
A. BCR-ABL testing
B. Bone marrow biopsy
C. Immunoelectrophoresis
D. JAK2 mutation testing
Answer and critique
The correct answer is B. Bone marrow biopsy. This item is Question 60 in MKSAP 18's Hematology and Oncology section. This older adult patient should undergo bone marrow biopsy. He has macrocytic anemia likely resulting from myelodysplastic syndrome (MDS), and a bone marrow biopsy will help confirm the diagnosis. The peripheral blood smear shows a dysplastic neutrophil with abnormal segmentation and hypogranularity and a nucleated erythrocyte, which are characteristic in patients with MDS. MDS is an acquired bone marrow failure syndrome with ineffective hematopoiesis and peripheral cytopenias. A bone marrow biopsy specimen showing hypercellular marrow with dysplastic myeloid progenitor cells and lack of orderly maturation is diagnostic. Bone marrow biopsy also helps with risk stratification of MDS, which determines treatment. Other causes of dysplasia, including chronic infections (HIV), vitamin B12 deficiency, alcohol use, and medications such as sulfamethoxazole, must be ruled out.
BCR-ABL translocation involving chromosomes 9 and 22 is pathognomonic for chronic myeloid leukemia (CML), a myeloproliferative neoplasm. CML typically presents in the chronic phase with elevated neutrophils or platelets, or both. CML cannot explain this patient's pancytopenia and abnormal peripheral blood smear findings.
Positivity for the JAK2 mutation is seen in certain other myeloproliferative neoplasms, such as essential thrombocythemia, polycythemia vera, and primary myelofibrosis. Primary myelofibrosis can present with cytopenias, but patients usually have other systemic symptoms, such as fever, night sweats, and malaise; findings of splenomegaly; and a peripheral blood smear showing teardrop erythrocytes and a leukoerythroblastic picture. This patient's clinical presentation with cytopenias and dysplastic neutrophils does not fit that of CML or other myeloproliferative neoplasms, so performing JAK2 mutation testing or polymerase chain reaction for BCR-ABL translocation is not necessary at this time.
Although patients with multiple myeloma may present with pancytopenia, anemia is more likely to be normochromic or normocytic and not megaloblastic as seen in this patient. Furthermore, patients with multiple myeloma do not have dysplastic leukocytes or nucleated erythrocytes in the peripheral blood.
Key Point
- Bone marrow biopsy can help confirm the diagnosis of myelodysplastic syndrome in patients with macrocytic anemia and other cytopenias and a peripheral blood smear showing dysplastic, hypogranular neutrophils, and nucleated erythrocytes.