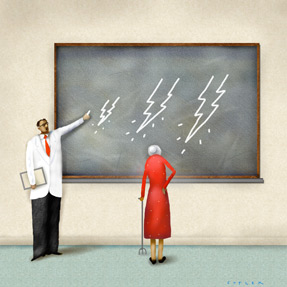
Spotlight cast on industry gifts, payouts to physicians
The Physician Payments Sunshine Act goes into effect Aug. 1. We detail what physicians need to know.
Next time a doctor is offered much more than a cup of coffee by a drug company or device manufacturer, the details are likely to be posted on a public website mandated by new, and sometimes confusing, federal provisions intended to bring all physician-industry relationships into the open.
The National Physician Payment Transparency Program (Open Payments) was passed in 2010 as the Physician Payments Sunshine Act, part of the Patient Protection and Affordable Care Act. A final rule was published in February 2013. It requires drug and device manufacturers and group purchasing organizations (GPOs) to start collecting data beginning Aug. 1 of this year.

Although it's becoming less common for physicians to receive gifts or other transfers of value from drug companies, many physicians still do so. The ACP Ethics Manual has addressed the issue directly, stating, “The acceptance by a physician of gifts, hospitality, trips, and subsidies of all types from the health care industry that might diminish, or appear to others to diminish, the objectivity of professional judgment is strongly discouraged. Even small gifts can affect clinical judgment and heighten the perception and/or reality of a conflict of interest.”
Information collected through Dec. 31, 2013, must be reported to CMS by March 31, 2014. CMS will begin posting the information on its public website Sept. 30, 2014, and will then update it annually each June 30.
Payments or other transfers of value of more than $10 per instance or $100 per year to physicians and teaching hospitals must be reported. Research is also included, as are textbooks that don't directly benefit a recipient's patients. Information on the website will include the recipient's name and address as well as the amount, date, form, and nature of payment and the name of the associated item.
Ownership or investment interests held by physicians or their immediate family members must also be reported. Public stock or dividends are exempted. The information will include the recipient's name and address, the dollar amount, value and terms of ownership or investment interest, and any payments or other transfers of value to physician owners or investors.
The payments then get placed in a category, such as consulting, gifts or honoraria. (See the sidebar “What will be reported” for details.)
Exclusions and exemptions
There are a number of exclusions that physicians should be aware of, but they can be confusing. Some have to do with accredited continuing medical education (CME). Attending accredited CME programs and speaking at them as faculty are excluded from reporting, said Neil Kirschner, PhD, ACP's senior associate for health policy and regulatory affairs.
Physicians need to be familiar with what does and doesn't qualify and know the details about specific CME activities. For example, attending the College-sponsored parts of ACP's annual scientific meeting won't be reportable, but attendance at an industry event without accreditation will be. A sit-down lunch at a symposium that's pharma-sponsored will be reportable. A buffet at a “large-scale” meeting where you can't tell who has eaten will not.
ACP is addressing these requirements and plans to make meeting attendees, and physicians more generally, aware of them, said Lois Snyder Sulmasy, JD, director of ACP's Center for Ethics and Professionalism. “Many collaborations with industry can advance the care of patients. But relationships can also introduce conflicts of interest that influence prescribing and utilization. ACP has long-standing policy on these issues,” she said. “So keep in mind that whether something is—or is not—reportable under the Sunshine Rule does not necessarily make it ethical.”
For example, residents are exempted from reporting, a provision that Ms. Snyder Sulmasy said is controversial. “ACP ethics guidelines about relationships with industry apply to residents, and we think applying these guidelines is especially important during training,” she said. (See the sidebar ““>Exemptions at a glance.”)
Despite this and other concerns, the College and experts are welcoming the new transparency.
Dr. Kirschner emphasized that the College has historically supported transparency to not only weed out inappropriate conflicts of interest but also to keep patients in the loop.
“People shouldn't view being on this website as a ‘list of shame’,” he said. “The fact that there is a relationship between industry and physicians is itself not a bad thing. ... It's appropriate for doctors to learn things, to consult, and to get grant money from industry. If it's out in the open it takes away the more nefarious potential or impression.” He also noted that having the information available publicly could increase trust between physicians and patients.
What's next
Some institutions, such as teaching hospitals, may already have strict annual reporting systems when there's a conflict of interest, but physicians still need to get ready for the change, advised Bernard Lo, MD, FACP, president of the Greenwall Foundation, a bioethics research institute based in New York City.
“I don't think doctors should be scared, but they should be prepared,” he said. “Anybody can look on the website—patients, neighbors, bloggers. It's not going to be easy the first time they say, ‘We hear you have aggregate payments from drug, device and biotech companies for X dollars. What's that all about?’”
Eric G. Campbell, PhD, professor of medicine at Massachusetts General Hospital and Harvard Medical School in Boston, guessed that the most likely parties to use the website will be journalists, nosy neighbors, relatives and lawyers. Researchers, too, he said, will want to see if taking a lot of gifts corresponds with utilizing expensive medicine at a higher rate.
“If analyses can show going out to dinner doesn't make the cost of care higher, then we can stop worrying about this stuff. But if it does and the doctor is benefiting personally from the drug company and the cost of that is borne by the American people in the form of higher drug costs—that's the Holy Grail for research,” he said.
Just having the information in the open will likely deter physicians from relationships between medicine and industry that don't pass the “sniff test,” said David Fleming, MD, MA, FACP, director of the MU Center for Health Ethics, chair of the department of medicine at the University of Missouri School of Medicine in Columbia, Mo., and ACP's 2013-2014 president-elect. He said the wide net cast by the $10 threshold will make everyone, not just the big players, think twice. “Most of us feel we're not influenced. But the reality is we are,” he noted.
The College recommends that physicians with investment interests or relationships with industry get familiar with what will be reported to avoid surprises. (ACP's guidance is online.
Other steps include the following:
- Register with CMS on the Open Payments website to access your personal data. Registration is by National Provider Identifier. Registration information will be made available later this year. Physicians also can subscribe to a CMS listserv that will send updates.
- Keep records of all payments and other transfers of value received from applicable manufacturers or GPOs.
- Once the data are reported, review the reports, experts strongly recommend. Physicians have 45 days to do so and submit requests for changes. All parties involved will have an additional 15 days to address disputed reports. Resolutions to disputes initiated during that time may not be reflected on the public website, however. Issues that aren't resolved will be marked as disputed, and resolved issues will be corrected when the data are next refreshed online. Payments will be listed by the date on which they are made, not according to when the event or service occurs.
The College encourages physicians to track transfers themselves. “If they have relationships with industry, physicians will want to protect their interests by doing their own independent tracking of investments, payments and other transfers of value to them that they can then check against company reports for accuracy,” Ms. Snyder Sulmasy said.
While the details still need to play out, experts said it's hard to argue anymore that patients shouldn't know the financial details of how physicians and industry interact.
“That's no longer tenable,” Dr. Lo said. “That's changed and I think that's changed forever.”