Alzheimer's, genomics and the personal utility of testing
As many as one in 10 doctors get asked for “the blood testâ€ï¿½ for Alzheimer's risk. A flurry of research will further drive patient interest, but also cause rethinking of clinical guidelines that discourage such testing.
Alzheimer's dementia strikes fear in the heart of elderly patients. It's not uncommon for older patients to present to clinic afraid that the groceries they forgot to pick up last week or the once-a-year lost car keys are a harbinger of the onset of the condition.
Recently, the mainstream media have given attention to genetic testing for Alzheimer's; occasionally patients request “the blood test” to predict their risk. Survey data suggest that a little over one in 10 primary care physicians have been asked to provide such testing. Anecdotally, I have been asked twice in the last month, a definite upswing from a few years ago.
The request for predictive genetic testing is not unreasonable from the patient's perspective. An estimated 60% of risk of developing Alzheimer's after age 60 is heritable, and about 25% of Alzheimer's patients have an affected parent. However, commercially available testing for the risk variant of the apolipoprotein E (APOE) gene ε4 has poor predictive value in asymptomatic individuals. Unsurprisingly, no major medical society endorses the use of APOE testing for screening purposes, and use of the test in a diagnostic setting remains controversial.
Testing for mutations causal of the uncommon forms of autosomal dominant early-onset familial Alzheimer's disorder is more predictive and less controversial, but only relevant to about 5% of all Alzheimer's cases. A flurry of high-profile research publications regarding late-onset Alzheimer's in the last few months will probably drive increased patient interest in testing and may cause some rethinking of professional guidelines that have discouraged it.
About 40% of Alzheimer's patients have at least one copy of the ε4 version of the APOE gene, and the same risk version is present in about 30% of the general population. Many individuals with the risk version never develop disease despite living to an advanced age, and some individuals with comorbidities die before the onset of clinically significant symptoms. Conversely, substantial numbers of individuals without the ε4 version of APOE develop Alzheimer's.
Many health professionals and behavioral scientists worry that APOE testing could result in psychological harms both because of the relatively poor predictive value of the test and because evidence-based options for risk reduction and therapy are limited. Others argue that such test results are empowering to certain individuals, and that patients are quite capable of dealing with ambiguity.
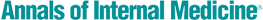
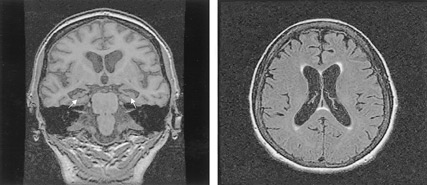
Two articles in the July 16, 2009 New England Journal of Medicine have added information to this debate. The first, by Caselli et al., demonstrated that some Alzheimer's patients harboring the APOE ε4 variant become detectably (but not necessarily functionally) impaired before age 60. This observation suggests that an earlier and expanded window of opportunity exists to spare neuronal damage and delay clinically important symptoms. Some health professionals argue that improved diet, exercise, smoking cessation and moderation of alcohol consumption might affect disease progression over time.
The second article, by Green et al., describes the REVEAL (Risk Evaluation and Education for Alzheimer's disease) study, in which children of affected individuals were randomized to receive or not receive personal APOE testing results under carefully controlled circumstances, and then followed longitudinally. Authors found little evidence for anxiety, depression or test-related distress up to one year out from disclosure.

Most in the genetics community have speculated that revealing a somewhat ambiguous risk for a devastating disease with little opportunity for risk reduction would cause substantial and potentially long-lasting emotional distress. The study by Green et al. suggests that such guidelines might be overly paternalistic.
In the last several months, genome-wide association studies have begun to yield new highly validated genomic risk markers. Variants in three genes were described by teams from the United Kingdom and France, each conferring a small but statistically robust risk for developing disease. The variants occur in or near the genes CLU, which encodes the brain apolipoprotein clusterin; PICALM, encoding a protein associated with synapse function; and CR1, encoding the complement component (3b/4b) receptor 1 protein. These proteins have previously been shown to be associated with biological processes potentially important to Alzheimer's dementia. These studies are the first to confirm a direct link with the pathological process in an unbiased way. Each discovery may provide a new approach to prevention and/or treatment, and perhaps improved risk prediction.
Taken together, recent research bolsters arguments made by proponents of the “personal utility” of APOE testing for Alzheimer's. Supporters argue that genomic testing can empower individuals to make healthy lifestyle choices outside of evidence-based medical models of care.
Personal utility as justification for genetic testing has arisen in the context of the direct-to-consumer genetic testing movement, often in the absence of controlled trials demonstrating clinical utility. Personal utility has appeal in an extremely fast-moving research and practice environment where trials demonstrating clinical benefits derived from testing may lag behind availability of the test by years, if not a decade. Despite the appeal, caution seems in order, particularly when the results might have a profound and poorly defined cascade of effects on patients and families.
Our understanding of Alzheimer's disease is rapidly expanding, fueled by advances derived from genomics and other disciplines of biomedical inquiry. It is highly likely that Alzheimer's risk prediction and management will improve considerably over the next decade, more closely aligning “personal” and clinical utility. Health professionals and guideline developers will need to monitor advances carefully and adapt as new insights for improved patient care emerge.